 This week’s Vital Signs report shows that antibiotics are being overpowered by lethal germs called carbapenem-resistant Enterobacteriaceae or (CRE).These germs cause lethal infections in patients that get inpatient medical care in hospitals, long-term care facilities and nursing homes.
This week’s Vital Signs report shows that antibiotics are being overpowered by lethal germs called carbapenem-resistant Enterobacteriaceae or (CRE).These germs cause lethal infections in patients that get inpatient medical care in hospitals, long-term care facilities and nursing homes.
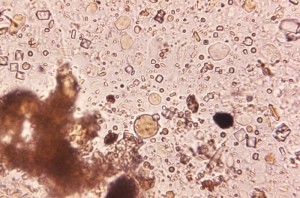
In their normal forms, the germs- in the Enterobacteriaceae family (e.g. E. coli) are a normal part of our digestive system. However, some of them have evolved and become resistant to all or almost all antibiotics we have today. When these germs get into the blood, bladder or other areas where germs don’t belong, patients suffer from infections that are difficult, and sometimes impossible, to treat.
Even though these infections aren’t common, their rise is alarming because they kill about 50% of people who get severe infections from them. In addition to causing lethal infections among patients, they’re especially good at giving their antibiotic-fighting abilities to other kinds of germs. This means that in the near future, more bacteria will become immune to treatment, and more patients’ lives could be at risk from routine bladder or wound infections.
Stopping these resistant Enterobacteriaceae will take a rapid, coordinated, and aggressive action that includes intense infection prevention work and antibiotic prescribing changes. You won’t be surprised to find that one of the primary lines of defense is that simplest of interventions called good hand washing by healthcare providers.
Other keys to effective prevention include making sure that antibiotics are prescribed wisely. Long term care facilities can also conduct Facility-level CRE Prevention that includes surveillance and facility-level prevention strategies that include core and supplemental measures. Here are some recommendations for facilities with no history of cases and a summary of prevention strategies for long-term care facilities.
CDC released a CRE prevention toolkit that puts together a clear set of control steps that facilities can take.












Amazing bacteria E. coli in our digestive system can be dangerous if they evolve! Thank you for this information, increase knowledge!
Thanks for sharing detail about bacteria.it is a very effective way and really informative article, Your article really usefull for me.
thank you Mr. Will..